Psychoneuroimmunology PNI
As mentioned by Andrawis A (2018), PNI psychoneurimmunology is an interdisciplinary new field of research that has emerged over the last 20 years and deals with the interactions of all body systems that are inextricably linked. There are various disciplines in this field, such as neurochemistry, neurophysiology, neuroanatomy, molecular biology, endocrinology, psychology, psychoanalysis and clinical psychosomatics. These disciplines have a common mood. This science is based on the fact that the body cells constantly communicate with each other and that the brain is also connected to the immune system.
The physical, mental and spiritual levels belong together. They are one unit and this was also experienced by early humans. This realization lives in the traditions of many cultures, it is also the basis of all great healing systems of the East. In orthodox medicine one cannot examine the human soul and its spirit with a scalpel and microscope (Andrawis A, 2018).
The human being is embedded in a network of different systems – the immune system, the hormone system, the nervous system and the psychosocial systems. Humans are not created as loners but are dependent on a social environment and thus live in social structures.
Ader, a pioneer in the field of psychoneuroimmunology PNI, coined this term (1975, 1982, Ader et. al. 1990), conducted a series of experiments on rats and tested the conditionability of the immune system. These experiments were often repeated and confirmed by clinical studies. For example, the immunosuppressive effect of glucocorticoids has been known for a long time and has been used by psychotropic drugs, but also other different substances, such as thyroid hormones, sex hormones and serotonin, which all have an influence on the immune system. The immune system is not always stable, but dynamic and highly sensitive in its function as defence. This is exactly why a research development in the PNI was developed. It is examined which cellular substances of the immune system are present, which play a special role in the investigation of social and psychological stress.
In earlier psychoimmunological studies, T (or B) lymphocytes were stimulated and their function was determined in vitro. Recently, deep layers of T lymphocytes and their interrelationships, the T4 helper cells, have been quantitatively identified. These cause the increase of immune defence and the production of antibodies. T8 suppressor cells have the ability to reduce immune response and autoimmunity disease. The task of T lymphocytes is to kill the cytotoxic infected cells. It is also interesting to continue research on “natural killer cells”. Why are the changes in the immune system caused by stress to be discussed?
This can be seen in the case of an imminent loss of a close relative, induced or experienced stress. It can lead to depression and social isolation. Various stressful life events lead to a weakening of the immune system. Several experiments with rats have also shown that psychological factors such as helplessness and hopelessness weaken the immune system enormously. Conversely, successful coping with stress has a very positive effect on health.
One can therefore conclude that psychotherapeutic or other “stress-reducing” aids strengthen the immune system and thus exert a positive influence on threatening or existing illnesses.
According to various follow-up examinations, psychotherapeutically treated patients become ill less frequently and go to the doctor less frequently (ibid.). Can the question be asked whether the immune system is autonomous?
Our immune system, which has become the focus of interest due to a variety of diseases, is the place where researchers discovered that it is part of a complex network. In the past, it was believed that the immune system was autonomous. Today we know that it interacts electrically with the psyche via nerve impulses as well as biochemically via neurotransmitters (messengers). This paradigm shift took place in the USA and coined the name psychoneuroimmunology.
The immune system is woven into the whole organism. The various immune cells that do their work for the body’s defence are created in the organs.
The PNI consists of four super systems
– Psychosocial System
– immune system
– hormonal system
– nervous system
7.1 The psychosocial system
This component plays a major role in the development of diseases.
Any psychological stress, be it stress-inducing situations or everyday experiences, as well as deficits in the social environment, material stress, fear of the future, family conflicts, social pressure, work stress, anger and rage, can trigger stress. This causes stress hormones such as cortisol and adrenaline to enter the bloodstream in elevated concentrations. This leads to various diseases. Those affected feel overwhelmed and at the mercy of their fate. The psychosocial systems have a negative interaction with the nerve-immune hormone system and thus lead to various mental illnesses (ibid.).
7.2 The Appearances of Psychoneuroimmunology PNI
As Deister has already described, PNI, whose pathological symptoms are very extensive, manifests itself in the form of cardiovascular disorders, intestinal complaints, sexual and pseudo-eurological symptoms, disorders of the digestive tract, palpitations,
Chest pain or other cardiopulmonary symptoms, nausea, abdominal pain, fatigue and other diffuse pain. It is only after many years that patients often only start therapy once they have noticed that their symptoms have not improved as a result of medical treatment (ibid.).
7.3 Psychosocial components
Psychosocial components influence the physical organ function up to physiological dysfunction. As Andrawis has already described, the differentiated opinion of the patient towards his physician in relation to the diagnosis complicates their dialogue. The patient’s conviction that these are only physical complaints, in contrast to the doctor’s diagnosis that a psychological, non-physical background exists, results in a conflict in communication due to the differences of opinion. The patient puts the main focus on getting attention. If the patients cannot convince their doctor of their own opinion, they react hypersensitively (ibid.).
Psychosocial stress
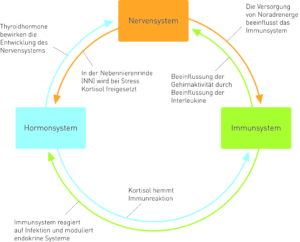
Fig. 6 Influence of psychosocial components on the organism Source: (Möller et al. 2005: 255).
7.4 The Nervous System, Hormonal System and Immune System
At Deter it is found that interpersonal relationships, as well as the emotional state itself, affect the immune system and are controlled by gene activity, as well as being influenced by immune messengers such as cytokines. The functioning of the T and killer cells of the immune system depends on how strong the immune system’s defence mechanism is (ibid.).
Fig.7 Cortisol – immune response – nervous system and hormone system
Source: (Fritzsche & Wirsching 2006:13)
7.5 Interactions of the four systems through stress
Stress reaction influences the interaction of these super systems and is connected with the development of mental and physical dysfunctions and thus affects the entire organism. One speaks of dysfunctionality of physiological cooperation (ibid.).
7.6 The Interaction of the Psychosocial System with the Immune System
The author points out that people are more likely to be affected by psychological disorders due to life-threatening conditions such as existential threats, loss of loved ones, divorce, separation, loneliness, as these psychosocial components have a negative impact on the body’s immunity, weakening the immune system, including the stress hormones cortisol, hyper-gonadotrope, hypogonadotrope and prolactin releasing hormone. If macrophages, the so-called killer cells, monocytes and lymphocytes are weakened, this may be a reason for reducing their function.
The immune system sends information such as interleukin 1 IL-1, cytokines, interleukin 6 IL 6, and tumor necrosis factor TNF to the nervous system. If the HPA axis activates cytokines, this may indicate a body infection.
If the T lympocytes are weakened, killer cells, macrophages and monocytes are also affected. This results in fatigue syndromes such as fatigue, aching limbs, insomnia, loss of appetite and listlessness, in this sense a pathological bodily dysfunction (ibid.).
7.7 Risk factors in psychosocial components
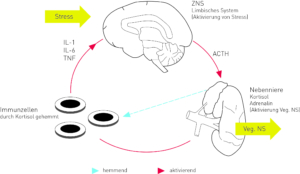
“With the concept of psychosocial risk factors, psychosomatic research has developed a model for the development and triggering of diseases that is equally valid for somatic, psychosomatic and psychological disorders” (Ermann 2004:21). The development of mental and physical illnesses is caused by a relation of psychosocial and genetic causes as well as childhood development and environmental pollution. There is an expression of conspicuous mental and physical states (ibid.) see Figure 8.
Fig. 8 Influence on immune system and central nervous system
Source: (Fritzsche & Wirsching 2006:14).
7.8 Psyche and hormonal system
As Fritzsche et al. have described, the pituitary gland and hypothalamus are on the one hand responsible for the regulation of the body’s own functions, whereby hormones are released. On the other hand, the psychosocial components and everyday stress influence the sensory neurons, which are thus carried on via the central nervous system (CNS) and contribute to the control of the activity of the neuroendocrine and autonomic nervous systems. This leads to dysfunction of the hormonal system and causes physiopathological symptoms such as mental disorders (ibid.). When the hormonal balance is disturbed, an overproduction of glucocorticoids occurs, whereby hyperthyroidism can be defined. This results in depressive moods, concentration and anxiety disorders, from which the affected person suffers.
In addition, patients with dysfunction of the adrenal insufficiency show a pathological fatigue syndrome. When vegetative stress develops, the pituitary gland, the hypothalamus and the adrenal cortex axis are activated and hypercortisolism can be assumed (ibid.).
This leads to an increased risk factor in cardiovascular disease. In the case of cortisone deficiency, an immunomodulating effect indicates chronic fatigue syndrome (ibid.).
7.9 The Psyche and the Nervous System
As already described by Andrawis A, (20018), the brain reacts in two different ways to everyday stress. One is the immune system and the other is the endocrine system, whereby the corticotropin-releasing hormone CRH is released by the hypothalamus. The pituitary gland contains the neurohormone responsible for the formation of the adrenocorticotropic hormone ACTH, which was released by the CRH. The cell is inhibited by the release of the adrenal cortex hormone cortisol and the formation of interleukins 1,2 and 12 (ibid.).
A vegetative control between central nervous system CNS, cytokines, immune system IS, kidneys and adrenal glands Mark AGM can be called axis. The connected organs involved, as well as the CNS, are responsible for the regulation of the body’s own organisms during activation of the vegetative nervous system and the Neuropeptide.
7.10 Stress, emotions and hormones
“Be angry, be sweet” suggested a professor at Harvard University, when in 1911 Walter Bradford Cannon (1871-1945), considering the symptoms, explained that anger caused by a bright red head and swollen veins of anger represented the rising adrenaline level. According to Cannon, emotions such as fear and anger drive the blood levels of glucose as well as the blood level of adrenaline. His simple experiment was: A cat locked in a cage, then tested for stress with a released and loudly barking dog, would then, hissing, show its claws, resist its hair and make the proverbial cat’s hump. Later, blood was taken from the adrenal glands with a previously implanted venous catheter, which showed more adrenaline than a blood sugar level above normal.
All this is due to the small side effect in which the hypothalamus, a part of the brain that is barely the size of an olive, apparently plays the main role, because it triggers an anxiety, escape or defence reaction in the event of an alarm and stages an adrenaline rush to counter the danger. Blood clots were removed from the blood by centrifugation in a small centrifuge and blood cells were pipetted into a physiological saline solution in which a cut piece of small intestine moved rhythmically. The movements stopped and the intestinal muscles slackened.
Signs with the adrenal hormone adrenal epinephrine were explainable by the release of the consequence that the adrenal gland has released the hormone adrenaline into the blood as a result of anxiety or anger. Cannon found less adrenaline than the angry cat’s blood in animals that were not angry or with those that were released or had their adrenal glands removed, as well as surprisingly a higher than normal blood sugar level. The administration of intravenous injections made another cat anxious and restless in another experiment. Not only did her blood sugar rise as sharply as in the first cat, she also excreted sugar in her urine. Untreated diabetes was diagnosed, recorded in the conspicuous symptom of glucosuria. Based on biochemical studies, we now know that muscles are inhibited, blood sugar rises and glucose is activated in the liver, providing energy in stressful situations (ibid.).
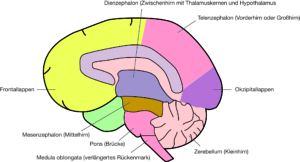
7.11 The Central Nervous System CNS
The left and right cerebral hemispheres of the cerebrum are surrounded by the meninges. They contain the right and left cerebral ventricles filled with cerebrospinal fluid, as well as the sympathetic nervous system and its opponent, the parasympathetic nervous system.
The sympathetic nervous system is activated by unconscious-emotional reactions during fighting and defence reactions, physical stress, as well as anger and anxiety.
Anatomy of The Nervous System
Fig. 9 Main sections of the brain source: (Rüegg 2003:3)
Thus, the cardiovascular system is also set in motion. All organs that are under the influence of the sympathetic nervous system also do so simultaneously under the influence of its opponent, the parasympathetic nervous system. This originates in the cruciate marrow, reaches the pelvic organs from there and runs through the spinal marrow to the brain stem. The most important parasympathetic cranial nerve is the vagus, the wanderer: It controls not only the heart, but the entire digestive tract. As the term “opponent” already suggests, the parasympathetic nervous system, unlike the sympathetic nervous system, leads to a recovery phase of the organism, which lowers heart rate and blood pressure. If there is harmony between sympathetic and parasympathetic nervous systems, the vegetative nervous system is in a balanced state. In unstable people suffering from vegetative dystonia, there is an excess of parasympathetic or sympathetic reactions. In the case of a pronounced sympathetic tone, nervousness prevails. In contrast, as already mentioned by Rüegg, an excess of parasympathetic activity leads to chronic fatigue – Chronic Fatigue Syndrome. The parasympathetic nervous system increases intestinal activity when it is disturbed by excessive sympathetic tone. If anger is suppressed, the parasympathetic nervous system can be inhibited. This can lead to constipation (ibid.).
Univ. Prof. Dr. Andrawis