Somatoform disorder
SSomatoform fault (ICD-10 V F45)
The somatoform disorders can be divided into three groups:
1 – Somatization disorder (pain disorder) (ICD-10 F45.0)
2 – Hypochondriac disorder (ICD-10 F45.2)
3 – Somatoform autonomic dysfunction / vegetative dysfunction
(ICD-10 F45.3)
(I will confine myself to these three disorders).
General information
Somatization disorders are multiform and the most common disorders. As already described in Tölle and Windgassen, they are diagnosed under different names. According to ICD-10 F45, somatoform disorders are classified as a generic term. Physical complaints exist without medical proof, but are to be seen in psychological-situational contexts. “Somatoform” therefore means “appearing in physical form”. (Tölle R, Windgassen K, 2009)
The main characteristics of somatoform disorders are described by the patients as physical complaints that cannot be attributed to an organ disease during a medical examination. In this disorder, as Deister points out, any organ can be affected. The consequences can be serious because there is a variety of different symptoms. Thus many examinations are necessary, possibly also in the consequence with operations. It often takes several years for the patient to visit a psychiatrist. Frequently, however, those affected do not see a psychiatrist. This leads to acute and chronic conditions. The somatoform disorder, also known as psychogenic disorder, requires a specific diagnostic and therapeutic strategy (Deister A, 2005).
Differential diagnosis
As already described by Dilling et. al., the differentiation from hypochondriac delusion is difficult due to the variety of symptoms. It is therefore helpful if the doctor knows the patient well and the patient has a good degree of self-knowledge. It is not disputed that the knowledge of the symptoms is perceived as unpleasant by the patient.
(Dilling H, Mombour W, Schmidt M H, 2008)
Appearance
Es gibt, wie schon Deister beschreibt, eine Vielfalt an Symptomen: Erschöpfung, Schmerzsymptome, Herz-Kreislaufbeschwerden, sexuelle und pseudoneurologische Symptome, Störungen des Verdauungstrakts (gastrointinale Beschwerden), Übelkeit und Unterleibsbeschwerden, Darmbeschwerden, kardiopulmonale Symptome (Herzklopfen oder Brustschmerzen) und andere diffuse Schmerzen.
Oftmals finden die Betroffenen erst nach mehreren Jahren den Weg zum Psychiater, da ihre organischen Beschwerden durch zahlreiche vorangegangene Untersuchungen und Operationen keine Besserung fanden. (Deister A, 2005)
9.3.1 Interrelation of Psychosocial Stress, Personality, Affectivity and Concept of Illness
Fig. 14: Interrelation of psychosocial stress, personality, affectivity and disease concept
Modified taken from: Möller H J, Laux G, Deister A, 2005, p. 255
In a broader sense, it is a difficult dialogue between patient and therapist. The patient is convinced of his organic complaints. He and his social environment usually do not know the causes. As already described by Dilling et. al., the attention-seeking (histrionic) behaviour of the patient is strongly pronounced. Those affected react sensitively if they are unable to convince the doctor of the disease as they see it (Dilling H, Mombour W, Schmidt M H, 2008).
Historical
Historical
In older diagnostic concepts and nosological systems, somatoform disorders have different names. The so-called “hysteria” was already known in ancient Greece. The term hypochondria was used to describe disorders that were suspected “under the ribs”. In the 17th century Sydenham related the two terms. Paul Briquet saw hysteria as a polysymptomatic disease in the middle of the 19th century. In recent decades, the most diverse terms such as “psychosomatic complaint complex”, “psychovegetative syndrome” and “vegetative dystonia” have been used with varying meanings.
(Deister A, 2005, p. 254)
Epidemiology
The number of new cases within one year is 13%. Women are 2:1 more likely to be affected than men. Of the patients in a General Hospital, 17-30% are affected by these disorders, about a third of them from a neurological department. As Frauenknecht and Brunnhuber have already explained, back and headache are the most common form of somatoform disorder. In two thirds of those affected, it occurs as comorbidity of their underlying disease, in particular depressive syndromes. A clear distinction should be made here between affective disorder and somatic symptoms, but there may also be a depressive episode with physical symptoms (“larviated depression”). At the same time, there is often a diagnosis of substance abuse / dependence, personality disorder, phobia, or panic disorder.
The somatoform disorder often occurs in adolescence and manifests itself in the third decade of life, but can also occur at any other age. A little later, the somatoform pain disorder almost always appears between the ages of 40 and 50. (Frauenknecht S, Brunnhuber S, 2008)
Aetiopathogenesis
It is assumed that different pathogenetic factors work together, e.g. unconscious conflicts in body language come to light in psychoanalytic procedures. In the neurobiological model, somatoform disorders are more common in first-degree relatives.
Reasons for the development of somatoform disorders:
– Identification with related parties concerned
– Self-insecure personality structures of affected persons
– Individual susceptibility of certain organs
– In case of over-strain due to stress, physical and mental strain over a longer period of time
– As Frauenknecht and Brunnhuber already describe, critical phases of life, physical illness or separation are often the trigger for somatoform disorders. (Frauenknecht S, Brunnhuber S, 2008)
Symptomatology
Fatigue is perceived as pleasant by healthy people. As Tölle and Windgassen describe it, exhausted people are hectic and tense and this is reflected in irritability, jitteriness, lack of concentration, poor performance, depression, mood swings, listlessness and a morose mood. In addition, there is a dizzy, unfree head, unsystematic dizziness, knocking headache, sleep disturbance, above all difficulties falling asleep, restless sleep, flickering in front of the eyes, fine trembling of the fingers, unpleasant sensation of accelerated pulse / extrasystoles, other heart complaints without organic findings, impotence, diarrhoea or constipation and stomach complaints. (Tölle R, Windgassen K, 2009)
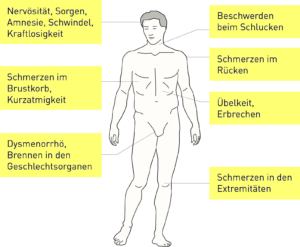
Various symptoms of somatoform disorders
Fig. 15: Various symptoms of somatoform disorders
Modified taken from: Möller H J, Laux G, Deister A, 2005, p. 256
Somatization disorder and symptoms
Somatization Disorder and Symptoms (ICD-10 F45.0)
differential diagnosis
Anxious and affective depressive disorders:
Anxiety and depression in varying degrees of severity are, as Deister already describes (Deister A, 2005), associated with somatisation disorders. You don’t have to make an extra diagnosis here. An additional diagnosis (anxiety/depression) only needs to be made in the case of a permanent condition that is in the foreground. After the age of 40, multiple physical symptoms indicate the onset of depression.
Physical disorders:
As already mentioned by Deister, in a chronic somatisation disorder it can be assumed that a physical disease develops over the years (e.g. hyperacidity/gastritis of the stomach later leads to a stomach ulcer).
– Refusal of the patient to accept the advice and insurance of the doctors to be healthy. The existing symptoms are not based on any physical diseases.
– The conviction of the presence of one or more diseases, despite numerous inconclusive investigations. Study of assumptions about the development of this disease.
– The duration of the disruption shall be at least six months.
– Despite organic inconspicuousness there are multiple physical symptoms.
– The behaviour resulting from this disorder affects the social and family environment.
– The appearance of the symptoms can refer to any part of the body as well as to any body system. (Deister A, 2005)
Somatisation disorder and symptoms after DSM-IV
Somatisation disorder and symptoms after DSM-IVPain symptoms
Headache, pain during urination, pain during sexual intercourse and menstruation, joint pain, chest or rectal pain and pain in the extremities, back pain and abdominal pain.
Sexual and gynaecological symptoms
Sexual indifference, irregular menstruation, often with increased bleeding, more frequent vomiting during pregnancy, ejaculation disorders, erectile dysfunction.
Pseudoneurological symptoms
Seizures, impaired balance or coordination, aphonia, dumpling in the throat, localized muscle weakness or paralysis, difficulty swallowing, urinary retention, blindness, numbness, seeing double images, hallucinations, pain sensation or loss of touch sensation.
Somatisation disorder
Somatization disorder (ICD-10 F45.0)
Over the years, there have been repeated and changing symptoms with the result of a complicated or often negative examination in various medical institutions. There have also been unsuccessful operations. As already described by Dilling et. al., the most frequently perceived gastrointestinal complaints are nausea, belching, vomiting, rumination and pain. Exceptional skin sensations can be seen in burning, tingling, itching, soreness, numbness and rash. Menstrual and sexual complaints are also common, as are anxiety and depression. The course of the symptoms is chronic and also influences the social environment. Patients become unable to work. The listed symptoms are more common in women than in men and usually begin in early adolescence. (Dilling H, Mombour W, Schmidt M H, 2008)
Diagnosis
– If multiple organic complaints are present for at least two years without medical findings,
– there is an impairment in dealing with society and the family as a result of the suffering and the resulting behaviour,
– the patient is convinced to be physically ill, he refuses to acknowledge mental causes and visits and examinations to various doctors are frequent.
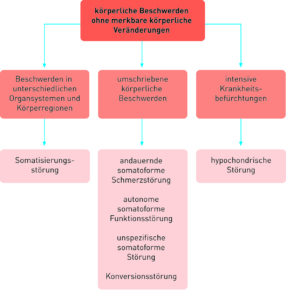
Model of a diagnosis of somatoform disorders
Fig. 16: Model of a diagnosis of somatoform disorders.
Modified taken from: Möller H J, Laux G, Deister A, 2005, p. 263
Hypochondriac disorder
Hypochondriac Disorder (ICD-10 F 45.2)
Differential diagnosis:
As Dilling et. al. already emphasize, the individuality of the symptoms and the recognition of the effects are important in this disorder. Attention must be paid to the presence of serious psychodynamics and its effects on disease. The patient attaches importance to extensive examinations (Dilling H, Mombour W, Schmidt M H, 2008).
The results should confirm the assumptions of the patient. Here the desire for a treatment to eliminate the symptoms is expressed. An exaggerated consumption of medicines can also be observed. The compliance during the therapy is missing. The patient mistrusts the prescribed medication and fears possible side effects. Nevertheless, he seeks reassurance in frequent visits to the doctor (Dilling H, Mombour W, Schmidt M H, 2008).
Appearance from a subjective point of view
As Deister has already described, the affected patients are persistently concerned with the possibility of being organically ill. Subjectively, the complaints are interpreted as exceptionally stressful. Those affected are excessively afraid of suffering from other diseases. The professional performance and social relations are affected by the constant concern with the complaints. “Doctor-shopping is part of the pattern of behavior of those affected. A constant change of doctor is part of everyday life. Finally, the referral to the psychiatrist is perceived as unpleasant and distressing. (Deister A, 2005)
The patient’s point of view
The patient is able to name his supposed disease more precisely (e.g. malignant tumor, stomach cancer, AIDS) and any physical discomfort confirms his opinion. After detailed examinations, these symptoms described by the patient are not confirmed by the findings.
As Frauenknecht and Brunnhuber already explain, the phenomenon of “Medical Student’s Disease” occurs in medical students especially in the clinical phase. Organic diseases are suspected, especially those that are currently the subject of study. The new medical knowledge brings with it an increased attention to one’s own body. (Frauenknecht S, Brunnhuber S, 2008)
Diagnosis Hypochondriac Disorder
Diagnosis Hypochondriac Disorder (ICD-10 F 45.2)
The hypochondriac disorder is characterized by extreme concern for one’s own body and by tantalizing fantasy images. In this case, it is not hypochondria as a disease, but the appearance of a syndrome.
Subjective sensations
The anxious attitude concerns worries about the urinary and sexual organs, gastrointestinal tract, heart, brain and spinal cord. As Tölle and Windgassen have already explained, fear and the resulting stress hormones cause a dysfunction of the vegetative nervous system. This also leads to an intensification of the hypochondriac symptom (circulus vitiosus). The patient’s extreme concern can be linked to actual physical organ symptoms. This hypochondriac malposition (overestimation) brings the patient’s tendency to a phobia into question. It should be noted that every human being has hypochondriac traits. However, hypochondriacs may also suffer from a serious disease. (Tölle R, Windgassen K, 2009)
Related terms:
– nosophobia
– dysmorphophobia
– bodily dysmorphic disorder
– hypochondria
– hypochondriac neurosis
(Dilling H, Mombour W, Schmidt M H, 2008)
Diagnosis hypochondriac disorder according to DSM-IV
– The patient’s occupation with his illness is taken seriously and the corresponding medical examinations are arranged. The results are inconspicuous and are confirmed by the doctor to calm the patient.
– Misinterpretation of the physical symptoms of people affected leads to excessive preoccupation with the idea of suffering from a serious illness.
Epidemiology
The majority of general practitioners and internists (Deister A, 2005) find disorders in their diagnoses, as Deister describes.
Somatisation disorder: This vegetative dysfunction affects women more frequently than men. In general hospitals, the proportion of people affected is between 20 and 40 %, in general practitioners’ surgeries about 10 % and in the general population about 4 %. The most common somatoform disorder is vegetative dysfunction.
Somatoform pain disorders: occur frequently in families and affect both men and women.
Hypochondriac disorders: affect 4-6% of the general population, they affect men and women equally.
Somatoform autonomic dysfunction
Somatoform Autonomic Dysfunction (Vegetative Disorder) (ICD-10 F45.3)
Patients describe their symptoms as purely physical manifestations. The fact is, however, that, as already described by Dilling et. al., the physical symptoms originate from the vegetatively (autonomously) controlled nervous system, cardiovascular, gastrointestinal and respiratory system. The urogenital system is also affected. The most common forms of complaint are disorders of the cardiovascular system (cardiac neurosis), the respiratory system (psychogenic hyperventilation) and the gastrointestinal system (diarrhoea and gastric neurosis).
In the diagnosis it is helpful to know two symptom groups which are not typical for organ symptoms.
The first group includes idiosyncratic, subjective and unspecific symptoms such as burning, tightness, severity, feeling of flowing pain or being pulled apart. The second group shows symptoms caused by stimulation of the autonomic nervous system such as tremors, flushing, sweating, heart palpitations.
These disorders are based on vegetative disorders. From the patient’s point of view, the illness of an organ is to blame for his complaints. The affected patients can often be attributed with psychological stress, problems and difficulties. (Dilling H, Mombour W, Schmidt M H, 2008)
Diagnosis
In order to make an accurate diagnosis, all these criteria must be fulfilled, as Dilling et. al. emphasize:
– No indication of an organ or organ dysfunction.
– Subjective sense of disease related to only one specific organ.
– Pathological adherence of the patient to the idea of having an organ disease, to be healthy despite the insurance of the doctor.
– Ongoing effects of vegetative stimulation such as flushing, sweating, palpitations and tremors. (Dilling H, Mombour W, Schmidt M H, 2008)
Therapy
Psychotherapies, especially cognitive-behavioral treatment approaches, are particularly effective in the treatment of body dysmorphic and hypochondriac disorders. For other disorders, this form of treatment is less effective. Positive effects can be observed in gastrointestinal and somatoform pain disorders.
Elements of a cognitive-behavioral psychotherapy / specific therapy program:
Relationship building:
As Frauenknecht and Brunnhuber already emphasize, it is important that the patient describes his complaints and the therapist listens attentively, expresses his appreciation and takes an emphatic attitude.
(Frauenknecht S, Brunnhuber S, 2008)
Motivation for therapy
Psychotherapeutic approaches explain to the patient the effects (e.g. muscle relaxation according to Jacobson to alleviate pain, important also stress reduction). Agreeing goals together.
Symptom management
Learning relaxation techniques (e.g. progressive muscle relaxation), distraction through these exercises, leading symptom diary to self-observation of symptoms.
Development of a general disease model
Accepting the suffering of the affected person through intervention (e.g. biofeedback methods, behavioral experiments, explaining connections between psyche and body through scientific methods).
Analyzing and Changing Dysfunctional Thoughts
keeping records of dysfunctional beliefs concerning the disease.
Reduction of social withdrawal and harmful behaviour:
The patient should be encouraged to find meaningful activities for him and to maintain social relationships again, to engage in sporting activities and to gradually assume responsibility at home and at work.
Stress reduction and motivation for joie de vivre:
Learning strategies to solve problems, building up hobbies, stress management strategies.
Organ-medical interventions and reduction of disease-related interactions
To instruct the patient to discuss the frequency and type of somatic interventions. The objective of this measure is the total omission of reinsurance.
Reduce drug abuse
Make the patient aware of the side effects of medication and point out the danger of dependence (e.g. long-term use of paracetamol for headache leads to a paradoxical effect).
(Frauenknecht S, Brunnhuber S, 2008)
Practical tips for psychosomatic treatments
– Observance of functional disturbances
– Avoidance of unnecessary investigations
– Acceptance of the patient’s complaints
– Precise therapeutic targets with formulation of sub-targets
– Avoid confronting the patient too early with psychological disorder models
– Cooperation and exchange of information with family doctor and therapists of other specialties
– Important: Motivation for therapy
Pharmacology
They lie, as Frauenknecht and Brunnhuber already describe, only few confirmed results are available for the drug treatment of somatoform disorders.
– Serotonin reuptake inhibitor in body dysmorphic and hypochondriac disorders with effective effect.
– Opipramol (tricyclic piperazinyl derivative, anxiolytic) in the treatment of somatoform autonomous disorder and somatization disorders.
– Low-dose tricyclic antidepressants (amitriptyline 10-75 mg) in the treatment of somatoform pain disorder. Neuroleptics and benzodiazepine preparations should be avoided because of their side effects (extrapyramidal motor symptoms, dependency development) (Frauenknecht S, Brunnhuber S, 2008)
Forecasting
The course of somatoform disorders is usually chronic. Spontaneous remissions rarely occur. The picture of social/occupational and physical disorders varies greatly from case to case.
Unfavourable forecast:
The following factors have negative effects: high secondary disease gain, clinging to the conviction of organic recovery, symptoms do not occur in connection with stressful or frightening experiences.
(Frauenknecht S, Brunnhuber S, 2008)
Favourable forecast:
From a psychoanalytical and behavioural therapy point of view, as Ermann describes, 65% of patients have the chance of a lasting improvement.
The results depend:
– the appearance of secondary processing
– the earlier the start of therapy, the better the chances of recovery (Ermann M, 2004).
From a psychoanalytical point of view
The analytical procedures involve various forms:
– Conflicts are dealt with, triggering strains are eliminated, psychotropic drugs are sometimes used in combination with imaginative procedures.
– Analytical group therapy can achieve good results because social conflicts and narcissistic traits within the group can be dealt with well.
– An inpatient stay is recommended in order to strengthen the motivation for treatment.
– The patient’s motivation for analysis is indispensable to reach the unconscious, as all causes of a disorder are suppressed as soon as they arise. In the course of this process, the patient recognizes his unconscious parts and accepts his problem and suffering.
– The patient should not only receive attention and care from his relatives. Pampering behaviour and compassion for the affected person as well as the satisfaction of neurotic needs support their syndromes and strengthen them.
– Family therapy should be considered prior to the actual treatment. (Ermann M, 2004)
– Personally, I am sure that recognizing and accepting suffering is the way to healing.
From the point of view of behavioral therapy
On the physiological level there are many applications, as already mentioned by Ermann (Ermann M, 2004):
– Biofeedback and stimulus overload, relaxation exercises, systematic desensitisation and cognitive restructuring, etc.
Tactile perception processes in somatoform disorders
Katzer A, Oberfeld D, Hiller W, Gerlach A and Witthoft M, from the Johannes Gutenberg University Mainz and the University of Cologne, show in their joint study (2011) the connection between tactile perception processes with somatoform disorders.
32 healthy and 33 participants with somatoform disorders were examined. The aim of the study was to determine whether the perception threshold is lower in persons with somatoform disorders than in healthy controls. The focus of the study was the sense of touch of the persons examined, namely the reaction time to a stimulus at the fingertips. An additional visual stimulus was given in the control group.
Through light stimuli an improvement of the tactile sense of both groups was achieved. This result was achieved in the second half of the test period. In the group of patients, there were indications of the effects of tactile perception and in particular of pseudoneurological symptoms. In the measurement of the group with somatoform disorders, the significance is lower with r= 0.86. Compared to the healthy group, the perception was positively confirmed. In the group with somatoform disorders, the distribution of symptoms is influenced by cognitive models (Katzer A, Oberfeld D, Hiller W, Gerlach A L, Witthöft M, 2012).
Univ. Prof. Dr. Andrawis